![]()
![]()
![]()
Use LEFT and RIGHT arrow keys to navigate between flashcards;
Use UP and DOWN arrow keys to flip the card;
H to show hint;
A reads text to speech;
38 Cards in this Set
- Front
- Back
|
What is the reading assignment for 0328110900 - GI E2 - Esophageal Dz (Yonts)?
|
Current
Diagnosis & Treatment Gastroenterology, Hepatology, & Endoscopy 2009 Pages 139-174 |
|
|
What are the "alarm signs" for GERD symptomlogy?
|
dysphagia, odynophagia (pain with swallowing), weight loss, persistent nause/vomiting, persistent symptoms despite tx, GI bleeding, advanced age, anemia, family hx of upper GI CA
|
|
|
What is the primary pathophysiologic causes of GERD?
|
inappropriate relaxation of the LES
|
|
|
What are the two main patterns of LES dysfunction?
|
1. Hypotensive LES (severe GERD, scleroderma)
2. Transient inappropriate relaxation (mild GERD, hiatal hernia) p139-140 |
|
|
What medications decrease LES pressure?
|
beta agonist, alpha blockers, anticholinergics, CCBs, diazepam, estrogen, narcotis, PRO, theophylline, TCAs
p140 |
|
|
What medications cause direct mucosal injury?
|
alendronate (fosomax), ASA, iron salts, NSAIDs, KCl tabs, quinidine, teracyclines (doxy)
p140 |
|
|
What foods exacerbate GERD symptoms?
|
Caffeine, chocolate*, peppermint*, EtOH* (red wine), soda, citrus, tomato, vinegar, large & fatty* meals, smoking*. * = decrease LES pressure
|
|
|
What lifestyle factors or medical factors exacerbate GERD symptoms?
|
weight gain, smoking, eating then lying down, pregnancy, scleroderma, immunocompromised, spinal cord injury
|
|
|
What are the symptoms of GERD?
|
Heartburn, regurgitation, dysphagia
|
|
|
How is GERD diagnosed?
|
1. tx with PPI, if pt improves, then dx = GERD,
2. if pt does not improve, scope or barium swallow |
|
|
What is reflux esophagitis and how is it treated?
|
Inflammation of the esophagus. Tx: lifestyle mods (diet, quit smoking, elevate head of bed, etc), H2-blocker/PPI, prokinetics, ABs, OMT, surgery, etc.
|
|
|
What is gastroparesis and what are the symptoms?
|
delayed gastric emptying not ass’d w/presence of an obstructing structural lesion in the stomach or distally in the GI tract. MCC = idiopathic, diabetic neuropathy, p-surgical. Other: Parkinson’s, collagen vascular disorders, intestinal pseudo-obstruction, paraneoplastic syndromes, SMA Syndrome, median arcuate ligament syndrome. Idiopathic = viral-like gastroenteritis, GERD, nonulcer dyspepsia, and cholecystectomy.
p201 |
|
|
What are complications of GERD?
|
bleeding from esophageal erosions/ulceration, stricture formation, Barrett’s esophagus, adenocarcinoma
|
|
|
How does H2 blockers and PPI’s work?
|
irreversibly block proton pump on parietal cells. H2 blocker: block H2 receptor on parietal cell – more AEs than PPIs
|
|
|
What is the most widely performed procedure for GERD, and what percentage of patients regain symptoms ten years after the procedure?
|
Nissen Fundoplication: fundus is wrapped 360 degrees around esophagus to promote LES closure. Last resort tx. Also used in tx of paraesophageal hiatal hernias. 80-90% sx free for 10yrs.
|
|
|
What is Barrett esophagus?
|
intestinal metaplasia in esophagus
|
|
|
How is Barrett esophagus diagnosed?
|
requires both visual (endoscopic) and histologic (biopsy) evidence
|
|
|
How is the gastro-esophageal junction (GEJ) identified?
|
Internal:
1. The squamocolumnar epithelial junction/Z-line (not in Barretts) 2. Transition from smooth epithelium to rugal folds. External: 1. Circular esophageal muscle fibers join oblique fibers of stomach 2. Gastroesophageal fat pad |
|
|
How is low grade esophageal dysplasia defined?
|
mucosal cells w/nuclei larger and hyperchromatic w/irreg. contours basally located in cell w/minimal-no stratrification..
|
|
|
How is indefinite grade esophageal dysplasia defined?
|
pathologist is not certain whether changes seen in the tissue are due to dysplasia. nuclear enlargement, crowding, hyperchromatism, prominence of the nucleoli, and mild stratification can be seen but are confined to the lower portion of the glands whereas the upper portion of the glands and surface epithelium show less abnormality or are normal.
P152 |
|
|
How is high grade esophageal dysplasia defined?
|
Distortion of gland architecture present/marked. Glands composed of branching and lateral budding of crypts and a villi-form configuration of mucosal surface. Dx requires loss of nuclear polarity and absence of consistent relationship of nuclei to each other.
|
|
|
What type of dysplasia has to be confirmed by 2 or more GI pathologists?
|
Any dx of high grade dysplasia
|
|
|
What is odynophagia?
|
painful swallowing
|
|
|
What are the two types of dysphagia and do the two types of dysphagia differ?
|
a. Oropharyngeal dysphagia - difficulty forming a bolus or initiating a swallow, nasal and oral regurgitation more common, commonly presents with general neuromusk. dz
b. Esophageal dysphagia - solids and liquids are problematic and symptoms localize in the chest and regurg, coughing and choking at night occur unrelated to swallowing, symptoms of GERD p155, 160 |
|
|
What symptoms suggest the patient is having oropharyngeal dysphagia?
|
difficulty controlling food in the mouth, inability to control food or saliva in the mouth, difficulty initiating a swallow, coughing, choking, frequent pneumonia, unexplained weight loss, gurgly or wet voice after swallowing, nasal regurgitation, and difficulty swallowing.
|
|
|
What causes cricopharyngeal achlasia?
|
persistent spasm/failure of UES relaxation
|
|
|
What are some of the primary and secondary causes of cricopharyngeal achlasia?
|
1* if confined to cricopharyngeus muscle w/o neurologic or systemic cause (idiopathic/intrinsic myopathy).
2* if by another disease process. |
|
|
What is a classic finding of cricopharyngeal achlasia?
|
cricopharyngeal bar on barium swallow – posterior wall of pharynx at level of cricoids cartilage.
|
|
|
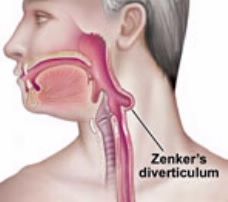
What is a Zenker diverticulum?
|
diverticulum in posterior wall of hypopharynx above cricopharyngeus muscle.
pic is just for reference |
|
|
What is a globus pharyngeus or globus sensation?
|
sense of lump in throat w/o dysphagia. often psychological.
|
|
|
What are the three components of esophageal peristalsis?
|
1. Inhibitory innervation dz – pregang vagus and post gang myenteric: relax LES and grade peristaltic contraction (VIP, NO).
2. Excitatory innervation dz – pregang vagus and post gang = basal LES HTN, HTN contraction and force of peristaltic contraction (ACh, Sub P). 3. smooth mm. dz: phasic muscles contract for peristalsis, tonic muscles = tone p159-161 |
|
|
What are the pathogenic causes of esophageal dysphagia?
|
motor/excitatory nerves – hypotonic muscles/LES. Enhanced contraction: HTN-LES, HTN-peristalsis. Disordered innervations: achalasia, DES
p160 |
|
|
What are the symptoms of esophageal motor dysfunction?
|
achalasia, DES, dysphagia, GERD, CP, regurgitation
|
|
|
What are the probable casues of esophageal chest pain?
|
hypertensive esophageal disorders, sustained longitudinal muscle contraction, esophageal hypersensitivity, and esophageal sensory neuropathy p163
|
|
|
What is achlasia?
|
thoracic esophagus dz of inhibitory innervation causing lack of esophageal peristalsis and incomplete relaxation of the LES
|
|
|
What is the preferred initial method of evaluation of dysphagia?
|
barium swallow
|
|
|
What are the symptoms of achlasia?
|
esophageal dysphasia to liquids and solids, chest pain, regurgitation
|
|
|
How is Eosinophilic Esophagitis dx'ed?
|
DIAGNOSIS REQUIRES > 20 ESOSINOPHILS PER HIGH POWERED FIELD
|

