![]()
![]()
![]()
Use LEFT and RIGHT arrow keys to navigate between flashcards;
Use UP and DOWN arrow keys to flip the card;
H to show hint;
A reads text to speech;
66 Cards in this Set
- Front
- Back
|
Compartment Syndrome:
Causes Presentation Treatment |
Rising pressure in muscle compartment impairs perfusion to compartment; can be due to fractures, crush injuries, burns, arterial injuries
Presentation: 6Ps Pain (hallmark) Pallor Pulselessness Paresthesias (most reliable sign) Poikilothermia (inability to regulate body temperature) Paralysis Treatment: Emergent decompression via fasciotomy |
|
|
What urinalysis abnormalities are indicative of UTI?
|
Leukocyte esterase
Nitrites |
|
|
What is the most common mechanism of injury for ankle sprain?
|
Plantarflexion and inversion
|
|
|
What is the most common mechanism of injury for MEDIAL ankle sprain?
|
Forced eversion and dorsiflexion (less common than lateral sprains)
|
|
|
History of a snap or tear is diagnostically significant in acute ____ injury.
|
Knee, not ankle
|
|
|
With regard to weightbearing, what sign is most suspicious for severe injury?
|
A patient who seeks help immediately and is non-weightbearing is more likely to have a severe injury than one who presents a few days after incident and is fully weightbearing
|
|
|
Which leg should be examined first when a patient comes in with injured leg?
|
uninjured leg before injured leg
|
|
|
What ligament is most likely to be injured in acute ankle injury?
What test allows for its assessment? |
Talofibular
Assess via anterior drawer test; if ligament is torn, talus will subluxate anteriorly |
|
|
Which ligament does the inversion test assess?
|
Calacaneofibular ligament; if ankle does not appear lax on inversion, ligament is intact.
|
|
|
Which ankle ligament is least likely to be injured?
|
Medial ligament
|
|
|
How are ankle sprains graded (I-III)?
|
Grade I: Stretching and/or small tear of ligament: slight to no fnal loss, mild tenderness, mild swelling, usually no ecchymosis, no mechanical instability
Grade II: Incomplete tear, moderate functional impairment, difficulty bearing weight, tenderness over involved structures, mild to mod pain, mild to mod swelling, ecchymosis common; moderate instability (stretching of joint with stress, but definite stopping point Grade III: complete tear and loss of integrity of ligament; inability to bear weight (unable to take four steps independently), severe swelling (greater than 4 cm about fibula), ecchymosis present, mechanical instability (significant stretching of joint with stress without stopping point) |
|
|
What is the most common acute ankle injury?
|
Lateral ankle inversion sprain caused by combination of plantarflexion and inversion
|
|
|
Differential for acute ankle injury
|
Sprain
Peroneal tendon tear (usually due to inversion injury or repetitive trauma) Talar dome fracture (may occur with ankle sprain, initial x-rays may miss; repeat imaging required is syx persist to detect avascular necrosis) Fibular fracture: due to falls, athletic injury, high velocity mechanism (MVA), inability to walk Tendonitits (usually posterior tibialis tendon) Subtalar injury: often due to high-energy injury |
|
|
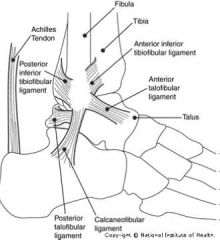
Draw ankle diagram with relevant tendons.
|
|
|
|
According to the Ottawa Rules, when are radiographs of the ankle needed?
Of the foot? |
Radiographs of ankle needed if:
There is pain in malleolar zone AND either: -bony tenderness along distal 6cm of posterior edge of malleolus OR -Inability to bear with both immediately and in ED Radiographs of foot needed if: -Pain in midfoot region AND -Bony tenderness in either navicular bone or base of fifth metatarsal OR -Inability to bear weight both immediately and in ED |
|
|
What is the RICE mnemonic for ankle sprain treatment?
|
Rest for first 72 hours only; not moving ankle for longer period of time can cause dec'd range of motion
Ice several times throughout day for 10 minutes at a time to reduce swelling/pain Compression with tape, elastic wrap, or semi-rigid ankle support (latter leads to quicker return to sports and work and less instability of ankle) Elevation to reduce swelling |
|
|
What anti-inflammatory medication can be given for acute ankle pain?
|
Ibuprofen 400-600 mg 2 to 3 times a day PRN
|
|
|
What ankle exercises should be recommended to patients with acute ankle injury?
|
Ankle inversion, eversion, plantarflexion, dorsiflexion
Calf-stretching, single-leg balancing |
|
|
How can patients avoid potential re-injury?
|
Avoid flip-flops or sandals and activities such as soccer until re-evaluation (usually 1 week)
|
|
|
Treatment for dysuria.
|
Bactrim or cipro if treating community with known high uropathogen resistance to TMP-SMX
|
|
|
How do the signs and symptoms of hyperthyroidism differ by age?
|
If under 50:
96% of pts present with tachycardia 96% increased sweating 92% heat intolerance 84% present with fatigue 84% tremor 50% with weight loss (also experience hyperreflexia, diarrhea, light tremors) If pts over 70: 71% tachycardia 56% fatigue Weight loss, atrial fibrillation Other typical syx are absent |
|
|
Why do patients with hyperthyroidism experience:
Tachycardia Weight Loss Exercise Intolerance and Fatigue |
Inc'd heart rate and cardiac output due to inc'd peripheral O2 needs and inc'd cardiac contractility (due to elevated T4)
Weight loss due to increased calorigenesis (heat produced by consumption of food), inc'd gut motility and associated hyperdefecation and malabsorption Exercise intolerance and fatigue contributed to by O2 consumption and CO2 production, respiratory muscle weakness |
|
|
Describe the hypothalamic-pituitary axis with regard to thyroid function.
|
Hypothalamus releases TRH
Pituitary releases TSH Thyroid releases T3/T4 T4/T3 exert negative feedback by controlling release of TRH/TSH |
|
|
What is the main cause of hyperthyroidism?
Pathophys? Triggers? |
Graves' Disease (toxic diffuse goiter);
Antibodies act at TSH receptor and stimulates gland to secerete excess T4/T3 Females 5-10 x more likely to have it than males Triggered by stressful life events, high iodine intake, recent pregnancy |
|
|
What physical exam finding is found in Graves' disease but not in other etiologies of hyperthyroidism?
|
Bruit/thrill seecondary to increased vascularity of thyroid
Pretibial myxedema secondary to increased deposition of hyaluronic acid in dermis/subcutis Exophthalmus (can be bilateral or unilateral)--up to 10% manifest when pt is euthyroid or even hypothyroid |
|
|
What symptom of Graves' will not resolve with radioactive iodine?
|
Proptosis
|
|
|
Based on age, which patients tend to have solitary/multinodular toxic thyroid goiters?
|
Younger patients (under 40) tend to have solitary toxic nodular goiter
Older patients (over 40) tend to have multinodular toxic goiters |
|
|
What causes hyperthyroidism after viral illness or pregnancy?
|
Thyroiditis; typically short term
|
|
|
What are the 2 main causes of excess iodine consumption? Effects?
|
Diet or amiodarone; may induce hyperthyroidism
|
|
|
Causes of thyroid goiter (enlarged thyroid gland).
|
Lack of iodine (most common cause worldwide)
Hashimoto's (causes hypothy) Graves Nodules Cancer Pregnancy Thyroiditis |
|
|
Signs and symptoms of hypothyroidism.
|
Weight gain
Cold intolerance Pedal edema Heavy periods Fatigue (common in both hyper and hypothy) |
|
|
Why is anemia on differential for palpitations?
|
Causes tachycardia via hypovolemia
Anemia can also cause dyspnea on exertion because of lack of O2 carrying capacity Common in women with heavy periods |
|
|
What lab value differentiates hypothyroidism from hyperthyroidism?
|
TSH
|
|
|
Diagnose:
High TSH Low T4 |
Hypothyroidism
|
|
|
Diagnose:
Mildly elevated TSH Normal T4 |
Subclinical hypothyroidism
|
|
|
Diagnose:
Normal TSH Increased T4 |
Pituitary adenoma (TSH-producing) or T4 resistance
|
|
|
Diagnose:
Decreased TSH Increased T4 |
Thyrotoxicosis (hyperthyroidism)
|
|
|
Diagnose:
Decreased TSH Decreased T4 |
Central (or pituitary) hypothyroidism (TSH and/or TRH deficiency)
|
|
|
Diagnose:
Decreased TSH Normal T4 Increased T3 |
T3 toxicosis
|
|
|
What are the cutoffs for a high vs low radioactive iodine uptake in a patient with suspected hyperthyroidism?
What do these values indicate? |
High RAIU (>30%): Graves if diffuse uptake, goiter, TRH-secreting pituitary tumor, HCG-secreting tumor
Low RAIU: <15%; subacute thyroiditis (gland leaking excess hormone, so uptake low bc more T4 not synthesized), silent thyroiditis, iodine induced, exogenous L-thyroxine, struma ovarii, amiodarone |
|
|
What antibody is detected in Graves' disease?
|
Thyroid peroxidase antibodies present in 70-80% of Graves' pts
|
|
|
Management of hyperthyroidism.
(Treatment and labs) |
Propranolol for syx relief of adrenergic symptoms (tachycardia, tremor, heat intolerance)
Pts with Graves' should be referred to opthalmologist Oral radioactive iodine (single dose) destroys overactive thyroid cells over few months; patients eventually become hypothyroid; must obtain pregnancy test! Check TSH every 2-3 months until stabilized; and every 6 mos thereafter. Alert pt to syx of hypothyroidism in advance |
|
|
Management of hypothyroidism.
|
Levothyroxine; adjust dose until patient feels normal and TSH is in normal range. Can be managed with 1-2 blood tests a year. usually stays about same.
Increase dose slowly; aim for dose of 1.5-1.8mcg per kg |
|
|
Criteria for diagnosis of diabetes.
|
1. HBA1c > 6.5% (do not have to be fasting)
2. Fasting glucose >126 3. Oral Glucose Tolerance Test (more sensitive, but difficult to do and poorly reproducible) 4. Random glucose >200 + syx of hyperglycemia Unless there are obvious syx of hyperglycemia, methods 1-3 should be confirmed by repeat testing |
|
|
Who should be screened for diabetes according to the American Diabetes Association?
|
Those with BMI over 25 and one or more of the following:
Habitual physical inactivity Minority (even Asian/Pacific Islander) First-degree relative with DM Previously dx'd impaired fasting glucose (100-125) or impaired OGTT (2-hour glucose 140-199) HTN (BP>140/90) HDL <35 or TG >250 Hx gestational DM, baby >9lbs PCOS Acanthosis nigricans Hx CVD IN ABSENSE of above risk factors, screening should begin at 45 years of age; if normal, repeat every three years |
|
|
Who should be screened for diabetes according to the USPSTF?
|
Asyx adults with sustained BP (treated or untreated) greater than 135/80
|
|
|
How is prevalence of neuropathy determined (physical exam finding)?
|
Loss of ankle jerk reflexes
|
|
|
What is fatalismo?
|
Holding to belief that control over one's diabetes is external to self, Latino patients may express that nothing can be done to improve their DM or health. "It is out of my hands" or "Everyone has to die from something"
|
|
|
Type 1 vs Type 2 DM:
Diabetic Ketoacidosis or Hyperglycemia Hyperosmolar State Serum pH Ketones (+/-) Serum glucose level |
DM I:
DKA pH <7.30 Ketones + Glucose >250 DM II: Hyperglycemia hyperosmolar state pH >7.30 Ketones - Glucose >600 |
|
|
Microvascular vs Macrovascular Complications (examples)
|
MIcrovascular: retinopathy, nephropathy, neuropathy
Macrovascular: CHD, cerebrovascular dz, peripheral artery disease) |
|
|
What are the components of a comprehensive diabetic foot exam?
|
Test for loss of protective sensation (monofilament plus vibration, pinprick, ankle reflexes)
Pedal pulses (dorsalis pedia and posterior tibial arteries); evaluates peripheral vascular dz--strongest risk factor for delayed ulcer healing and amputation in diabetes patients Inspection for breaks in skin, pressure calluses that precede ulceration, existing ulceration and infection, bony abnlts, hair loss, temp changes; examine footwear for abnlr patterns of wear and appropriate sizing |
|
|
What does HbA1c value reflect?
How often should it be performed? |
Reflects plasma glucose concentrations over 4-12 week period
Perform at diagnosis and at least twice a year in pts who are stable and <7% |
|
|
Most diabetic patients will die from ___________.
|
Cardiovascular disease
|
|
|
Why should B12 levels be measured in diabetics?
|
Metformin can cause asymptomatic subnormal levels of B12; only perform if pt exhibits neuropathy
|
|
|
When should TSH be performed in diabetics?
|
If patient has DM1
|
|
|
What labs should be ordered at baseline DM visit?
|
HbA1c
EKG Spot urine albumin:creatinine ratio Fasting Lipid Profile (dyslipidemia can complicate management of DM) |
|
|
What is the 1st treat treatment algorithm for DM II?
|
1) Diagnosis: If HbA1c >6.5%: lifestyle changes plus metformin
2) Assessment: If HbA1c >8%: continue lifestyle changes and metformin; add sulfonylurea (Glyburide, Glipizide, Glimepiride) or basal insulin (glargine, detemir, NPH) 3. Reassessment: If HbA1c >8: continue lifestyle changes and meformin, add basal insulin or intensify insulin regimen. Consider discontinuing sulfonylurea to avoid hypoglycemia. Can move on to step 4, but this is 2nd tier (fewer well-validated studies support this approach): Adding rapid-acting insulin with meals Thiazolidinediones--Glitazones (Actos) or rosiglitazone (Avandia) for those who can't tolerate GI f/x of metformin or have hypoglycemia w/sulfonylureas GLP-1 analogs: exenatide, liraglutide Etc. |
|
|
What is the target for HbA1c? Why?
|
HbA1c under 7% prevents microvascular disease (retinopathy and nephropathy)
However, blood pressure and lipid control demonstrate more improvement of CV risk than intensive glycemic control. |
|
|
Goal for fasting blood glucose?
Postprandial glucose? |
80-120 fasting
<180 postprandial |
|
|
What are the preferred HTN drugs for diabetics?
|
If BP >140/90
ACE inhibitor, ARB, beta blocker, or CCB; plus lifestyle change (reduce CV events and risk) |
|
|
What are the LDL goals in patients with diabetes?
|
If no known CVD, <100 mg/dl
if known CVD using statin, <70 mg/dl |
|
|
When should aspirin therapy be used in patients with diabetes?
|
history of CVD or at moderate/high risk of CVD
Common dose is 81mg qd No e/o use of ASA in pts under 30; contraindicated in pts <21 bc of Reye's If have CVD and an ASA allergy, use clopidogrel 75 mg qd |
|
|
Advise all patient that smoke to ______.
|
Quit, not just cut back!
|
|
|
What risk does smoking pose in patients with diabetes?
|
higher risk of premature development of microvascular complications and CVD. Smoking is most important modifiable cause of premature death.
|
|
|
Recommended eye care for diabetics.
|
yearly dilated ophtahlmoscopic exam as many pts w/retinopathy may not complain of syx
|
|
|
What immunizations are recommended for diabetics?
|
Annual vaccination for influenza
Pneumococcal vaccine for diabetics > 2 years; one-time revaccination for patients over 64 if received first dose more than 5 years ago Should also receive revaccination if have nephrotic syndrome, chronic renal disease, or are immunocompromised |

